INTRODUCTION
Definitions
- Spondylolisthesis:
- Forward displacement of 1 vertebra on another
- Usually L5-S1 in isthmic & L4-L5 in degenerative spondylolisthesis
- Spondylolysis:
- Defect in pars interarticularis
- Present in about 5 to 6% of adult population
- Spondyloptosis:
- >100% slip
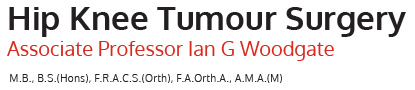
Classification (Wiltse)
- Type I:
- Dysplastic
- Congenital anomalies of upper sacral facets or inferior facets of 5th lumbar vertebra that allow slipping of L5 on S1
- No pars interarticularis defect is present in this type
- Type II:
- Isthmic
- Defect in pars interarticularis that allows forward slipping of L5 on S1 (> L4 on L5)
- 3 subtypes
- Lytic (stress fracture)
- Elongated (but intact)
- Acute fracture
- Type III:
- Degenerative
- Lesion results from intersegmental instability of long duration with subsequent remodelling of articular processes at level of involvement, esp L4/5
- Type IV:
- Traumatic
- Results from fractures in area of bony hook other than pars, such as pedicle, lamina, or facet
- Type V:
- Pathological
- Results from generalised or localised bone disease & structural weakness of bone such as osteogenesis imperfecta, tumour infiltration
- Type VI:
- Iatrogenic
ISTHMIC SPONDYLOLISTHESIS
Epidemiology & Natural History
- Hereditary predisposition
- Begins during childhood, however most patients do not seek medical attention until adulthood
- 75% of defects radiographically evident by 6 years of age & 75% of patients with spondylolysis also demonstrate spondylolisthesis
- Onset of symptoms tends to occur after childhood with a mean age at presentation of 20 years
- Slip >10mm correlates positively with symptoms
- Foraminal stenosis occurs in as many as 75% of patients & may be, but is not always, associated with leg pain or radicular symptoms
Clinical Manifestations
- While subjective complaints of leg pain are common, documented neurologic deficit or radiculopathy is seen less frequently (16 to 27% of cases)
- Subjective decrease in light-touch sensation over dorsum of foot & mild weakness of EHL are most common neurologic abnormalities, correlating with L5 root irritation as seen with L5-S1 spondylolisthesis
- Straight leg raising is usually normal
- Loss of bowel & bladder function does not routinely manifest
Imaging
- Plain radiographs:
- AP & lateral views (preferably standing)
- Oblique projections to highlight pars & 30° caudal-tilt AP view
- Classification (Meyerding Severity Scale – based on S1 width)
- Grade I - 0 to 25%
- Grade II - 25 to 50%
- Grade III - 50 to 75%
- Grade IV - 75 to 100%
- Grade V - >100% (spondyloptosis)
- CT:
- Bony anatomy
- MRI:
- Thecal sac compression in high grade deformity
Predictors of Progression
- Young age
- Female
- Dome shaped upper S1 end-plate
- Sacral inclination >30°
- Slip angle >10°
- High grade slip (III+)
Principles of Management
- Non-operative:
- Simple analgesics & NSAIDs
- Activity modification
- Physiotherapy
- Strengthening exercises
- Postural retraining& correct lifting techniques
- Smoking cessation
- Anti-lordotic bracing
- 83% good to excellent results at 7 years
- Operative:
- Indications
- Persistent or intolerable leg or back pain
- Progressive deformity
- Worsening motor deficit, including foot-drop & bowel or bladder dysfunction (extremely rare)
- Arthrodesis
- For patients who have persistent complaints of lower back pain, with or without radiculopathy, & who have not responded satisfactorily to non-operative management, arthrodesis may be indicated
- Patients with spondylolisthesis tend to fare better than patients who undergo arthrodesis for other reasons (>90% success)
- Surgical approach
- Wiltse approach (parasagital between multifidus & longisimus; enables direct line for pedicle screw insertion)
- Posterolateral fusion with bone graft in lateral gutters & pedicle-screw & rod instrumentation
- For patients with a slip of <50% & a normal or near-normal adjacent disk, single-level fusion is used
- If spondylolisthesis is >50%, or if there is significant disc degeneration just above level of slip, extension of fusion to next level is undertaken
- Full return to strenuous work & recreational activity is usually not possible before 6 months, i.e slow post-op course
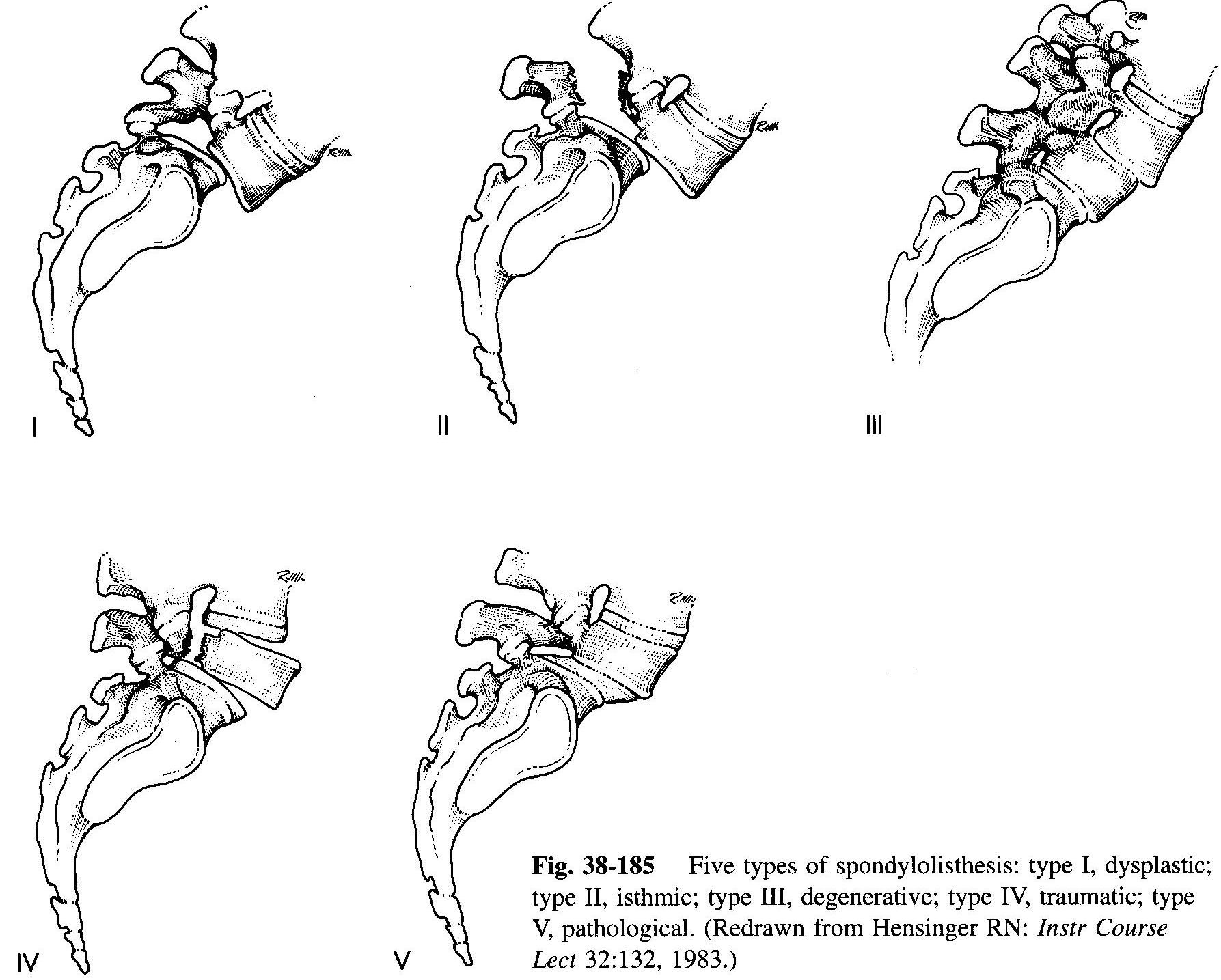
- Decompression
- Neural foraminal narrowing with associated nerve-root compression & leg pain is common in adults with isthmic spondylolisthesis
- Gill procedure (excision of the loose posterior arch) + lateral nerve-root release by foraminotomy to adequately decompress affected root
- Limited decompression, consisting of generous foraminotomy, with resection of interposed fibrocartilaginous material from pars defect while retaining the lamina is an alternative
- Indication for formal decompression
- Presence of an objective neurologic deficit, including significant radicular pain or nerve-root dysfunction nerve-root irritation (pain, numbness, or sensory loss without associated motor involvement) or nerve-root compression (radiculopathy &/or motor loss)
- Patients with leg pain, but without objective deficit, benefit from fusion without decompression
- Reduction
- Indications
- High-grade spondylolisthesis with significant lumbosacral kyphosis (increased slip angle) resulting in an unacceptable deformity &/or a mechanically unfavourable position of L4 relative to sacrum for fusion
- Mean obtainable slip correction 90%
- Complications
- Loss of reduction
- Failure of fusion (up to 33%)
- Neurologic deficit, most commonly L5 root injury which is manifested clinically as foot-drop (up to 20%); thorough root decompression, slow reduction of slippage, & intra-operative neurologic monitoring lessen risk of neurologic injury
- Indications
- Indications
DEGENERATIVE SPONDYLOLISTHESIS
Epidemiology & Aetiology
- Women more commonly affected than men
- Prevalence increases with age
- Diabetic patients & women who have undergone oophorectomy at greater risk
Pathophysiology
- Most important requisite for degenerative spondylolisthesis is relative immobility of lumbar segment below lesion
- Immobility most commonly due to hemi-sacralisation (Bertolotti’s syndrome) but can also result from advanced disc degeneration at the L5-S1 level
- This finding is thought to have etiologic significance because immobility of L5-S1 level shifts mechanical stresses to adjacent L4-5 level
- An iatrogenic cause for immobility is spinal fusion
- Forward slip occurs many years after original fusion; surprisingly, many patients are asymptomatic despite the deformity
Differential Diagnosis
- Osteoarthritis of hip
- Sacroiliac pathology
- Degenerative scoliosis:
- In these patients neurologic complaints may be more diffuse, consistent with multi-level involvement
- Diffuse idiopathic skeletal hyperostosis (DISH):
- Characterised by multi-level bridging osteophytes
- Commonly affects middle-aged & older men
- Diabetes & hyperuricaemia
- Cervical spinal stenosis
- Intrinsic neurologic disorders
- Primary or metastatic disorders
- Peripheral vascular disease:
- A useful differentiation is that patients with a spinal cause usually are relieved of symptoms only by cessation of walking & sitting down or flexing the spine
- In contrast, patients with a vascular cause have only to stop walking & symptoms disappear in normal upright standing position
Clinical Signs & Symptoms
- Back pain:
- Episodic & recurrent for many years
- Worsens over course of day
- Radiation into posterolateral thighs
- Mono-radiculopathy is less common type of leg pain:
- When present, it is result of entrapment of L5 root in lateral recess.
- More common pain presentation is that of neurologic claudication:
- Pain may be diffuse in lower extremities, involving L5 &/or L4 roots unilaterally or bilaterally
- Accentuated by walking & relieved by forward flexion of spine
- Additional complaints include cold feet, altered gait, & “drop episodes,” where patient unexpectedly falls while walking
- With extreme stenosis, interference with bladder & bowel control can occur
- Unlike acute & often devastating bladder & bowel symptoms of cauda equina syndrome in lumbar disc herniation, spinal stenosis often has an insidious & subtle presentation
- Stenotic symptoms are result of mechanical & vascular factors
- As slip progresses, facet hypertrophy, buckling/infolding of ligamentum flavum, & diffuse disc bulging contribute with forward displacement to compression of cauda equine
- Relief of symptoms that follows forward spinal flexion is thought to be related to increase in AP dimensions of spinal canal
- At extreme, patients may report need to sleep in foetal position to relieve leg symptoms
- Significant vascular component in complaints of leg pain may lead to another manifestation, restless legs syndrome
- In this condition, patients are awakened by aching pain in calves, restlessness, an irresistible urge to move legs, & fasciculations
- Exacerbated by congestive heart failure
- Numbness & weakness, are variably present
- Some patients present with degenerative spondylolisthesis above a spinal fusion
- A long symptom-free interval is followed by onset of nerve-root symptoms & stenosis emanating from level above their previous fusion
Physical Examination
- · Loss of lumbar lordosis
- When stenotic symptoms are severe, a fixed forward-flexed posture, sometimes accompanied by hip-flexion contractures, can be observed
- Except in very thin patients, step deformity usually is not palpable
- Normal spinal mobility or hypermobility
- Commonly, neurologic findings are nonspecific & may include bilaterally absent reflexes, spotty sensory losses, & muscle atrophy without frank weakness
- When bladder symptoms are reported, sensory loss may be present in perineal area, accompanied by a decrease in rectal sphincter tone
Imaging
- Plain radiographs:
- Disc-space narrowing, vacuum sign, endplate sclerosis, peridiscal osteophytes, & facet sclerosis & hypertrophy +/- hemi-sacralisation of L5
- Dynamic flexion-extension radiographs
- Instability in flexion-extension is displacement exceeding 5 mm.
- CT:
- Use of reverse gantry imaging to exclude any possible pars defect
- MRI:
- Indications
- Significant & progressing neurologic claudication or radiculopathies
- Clinical suspicion that another condition, such as metastatic disease, may be causative
- Bladder or bowel complaints
- Findings
- Constriction of cauda equina associated with a diminished cross-sectional area & diameter
- Facet degeneration & hypertrophy with subarticular entrapment of L5 nerve roots
- Apparent thickening & buckling of ligamentum flavum, & diffuse disk bulging
- Indications
Management
- Non-operative:
- NSAIDs
- Physiotherapy
- Weight reduction
- Management of osteoporosis
- Epidural blocks
- Operative:
- 10 to 15% of patients are surgical candidates
- Indications
- Cauda equina dysfunction, accompanied by evidence of a complete block at affected level
- Progressive muscular weakness of functional significance, such as a dropped foot or quadriceps dysfunction
- Progressive & incapacitating radicular pain or claudication, particularly when it causes sleep disturbance
- Failure of non-operative management
- Procedure
- Decompressive laminectomy
- Disc should not be excised unless it is frankly ruptured (excising disc increases risk of later instability)
- Following decompression, patency of dural sac is established by presence of dural pulsations & absence of nerve-root tension
- Fusion
- Indicated when adequate decompression requires sacrifice of >50% of facets or when pars has been breached
- May be necessary to extend fusion to L5-S1 level in patients, unless that level is stabilised by bone abnormalities or marked disc degeneration
- Results
- 70 to 85% success rate for treatment of radiculopathy or claudication
- Relief of low back pain is less predictable
- Predictors of failure are increased age, associated comorbidities (e.g. cardiac disease), & a longer duration of surveillance